What are pneumatized mastoid air cells?
Pneumatization begins early in childhood and continues until adulthood. The mastoid bone is located behind the ear and is connected to the middle ear through the mastoid antrum. Air cells develop as the mastoid bone grows, forming a complex network of interconnected spaces. These air cells are filled with air and are lined with a thin layer of mucous membrane.
The pneumatization process is essential for proper ear function. The air cells help to ventilate the middle ear and regulate pressure. This is important for hearing because it allows sound waves to travel efficiently through the ear canal and middle ear. The air cells also help to protect the middle ear from infection.
Pneumatization can be affected by various factors, including genetics, infection, and injury. Mastoiditis, an infection of the mastoid bone, can occur if the air cells become blocked or infected. This can lead to inflammation, pain, and even hearing loss. However, in most cases, pneumatization is a normal and healthy process.
What is the theory of Pneumatization of the mastoid?
Let’s dive a little deeper into this theory. Imagine a healthy middle ear: It’s like a small, well-ventilated room with a doorway (the eustachian tube) that connects it to the outside world. When this door is open, air can easily move from the back of your nose and throat into the middle ear. This airflow plays a key role in shaping the mastoid. The constant flow of air pushes against the bony walls of the mastoid, gradually carving out those air pockets.
However, if the doorway gets blocked – like when you have a cold or allergies – the air pressure inside the middle ear can’t equalize with the air pressure outside. This can lead to a buildup of fluid, which can irritate and inflame the middle ear lining. Over time, this inflammation can affect the process of pneumatization, preventing the mastoid from developing its air pockets. It’s like trying to build a house with a blocked door – you can’t get the materials in to finish the construction.
So, according to Wittmaack’s endodermal theory, a healthy middle ear lining is essential for normal mastoid pneumatization. If the lining is compromised, it can disrupt the flow of air and affect the development of those air pockets.
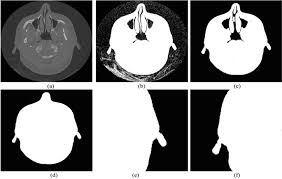
What are the types of mastoid Pneumatization radiology?
Pneumatic: This type represents full air cell development within the mastoid bone, indicating a healthy and well-pneumatized mastoid.
Sclerotic: This type signifies a solid bone mastoid, lacking air cells, potentially due to previous inflammation or infection.
Diploic: This type exhibits a marrow-filled mastoid bone, with no air cells.
Mixed: This type presents a combination of air cells and marrow, indicating a partially pneumatized mastoid.
Understanding these types helps radiologists interpret imaging studies, which is crucial for diagnosing and managing conditions affecting the mastoid bone.
Let’s delve deeper into each type:
Pneumatic: A pneumatic mastoid is considered the ideal type, offering several advantages. It provides a buffer against infection, as the air cells act as a protective barrier. Additionally, it aids in sound transmission by contributing to the middle ear’s resonance properties. This type is commonly seen in healthy individuals.
Sclerotic: A sclerotic mastoid can arise from chronic infections or inflammation, resulting in the replacement of air cells with dense bone. This type can make it challenging to distinguish between normal bone and disease processes, requiring careful evaluation.
Diploic: In a diploic mastoid, the bone marrow fills the mastoid cavity instead of air cells. This type is less common and is often associated with certain genetic conditions.
Mixed: A mixed mastoid, as the name suggests, exhibits a combination of air cells and marrow. This type is often observed in individuals with previous infections or inflammation that may have partially disrupted the pneumatization process.
Remember, it’s important for radiologists to accurately identify the type of mastoid pneumatization to make informed clinical decisions. It’s also crucial to understand that the degree of pneumatization can vary within an individual’s mastoid bone, even within the same ear. This variability makes it essential for radiologists to carefully analyze the images and consider the patient’s history when interpreting the findings.
At what age are mastoid air cells aerated?
The mastoid bone, located behind the ear, is filled with air cells that connect to the middle ear. This process of air cell development is called pneumatization. Pneumatization begins slowly after birth and continues until adulthood.
The air cells help to lighten the skull and improve hearing by reducing the pressure in the middle ear. As the cells grow, they create a network of interconnected spaces within the mastoid bone. This process is essential for proper ear function and can be affected by various factors, including ear infections and genetic predisposition.
The development of mastoid air cells is a gradual process. It’s important to understand that this process can vary slightly from person to person, and the age of complete pneumatization may also vary. However, it generally occurs before the age of six.
What is the meaning of Pneumatization?
Firstly, pneumatization helps lighten the weight of the bone. Imagine carrying around a heavy, solid skull all day – not very efficient! By creating these air pockets, the bone becomes less dense and easier to move around.
Secondly, these air-filled cavities can help with sound resonance. Think of how a hollow tube can amplify sound. In our skulls, pneumatized bones can help with hearing and speech by resonating sound waves. This is especially important for the bones around our ears and sinuses.
You can even find pneumatization in other areas of the body, like the sinuses in our face, which are air-filled spaces that connect to our nasal cavity. They’re actually pretty important for helping drain mucus and keep the nasal passages clear.
Is pneumatization normal?
Imagine your sinuses like empty rooms in your skull. As you grow, these rooms get bigger. Air fills those spaces and that makes breathing easier, especially when you have a cold or allergies. The process of pneumatization is like building more space in those rooms to give your sinuses room to grow.
Now, even though pneumatization is normal, there are times when it can happen a bit more than usual. This is called hyperpneumatization. Think of it like having a really big room in your skull. While it’s not necessarily a bad thing, sometimes it can lead to problems like sinus headaches or infections. If you have any concerns about sinus pneumatization, it’s best to talk to your doctor. They can tell you if everything is normal or if there’s something else going on.
What is the role of mastoid Pneumatization in temporal bone fractures?
Imagine the temporal bone as a sponge – the mastoid air cells act as small, interconnected spaces filled with air. These air cells contribute to the pneumatization of the mastoid, giving it a porous structure. When direct lateral trauma occurs, the kinetic energy is absorbed by the mastoid air cells, like a sponge absorbing water. This disperses the energy, reducing the force transmitted to the surrounding bone and decreasing the chances of a temporal bone fracture. Think of it like a punch landing on a pillow instead of a solid wall – the pillow absorbs the impact and reduces the force transmitted to your head.
The extent of mastoid pneumatization can vary greatly between individuals. Some people have a very well-pneumatized mastoid, with many large air cells, while others have a less pneumatized mastoid with fewer and smaller air cells. The level of pneumatization can impact the ability of the mastoid to absorb and disperse energy during trauma. A well-pneumatized mastoid offers greater protection against fracture. In contrast, a less pneumatized mastoid might be more susceptible to fractures in cases of direct lateral trauma.
Are paranasal sinuses and mastoid air cells Pneumatized?
Let’s break this down a bit. Pneumatization is basically the process of filling up spaces with air. Think of it like blowing up a balloon – you’re inflating it with air. In the case of the mastoid air cells and paranasal sinuses, this process starts during fetal development and continues throughout childhood.
Mastoid air cells are located in the mastoid bone, which is behind the ear. They are connected to the middle ear, which helps to regulate pressure and drain fluid. Paranasal sinuses are located in the skull, surrounding the nasal cavity. They are also connected to the nasal cavity and help to humidify and warm inhaled air, as well as reduce the weight of the skull.
Why are these spaces pneumatized? There are a few reasons:
Weight reduction: Filling these spaces with air helps to make the skull lighter, which is important for balance and mobility.
Sound resonance: The air-filled spaces in the sinuses and mastoid cells can contribute to sound resonance, which is important for speech.
Protection: The air-filled spaces can help to protect the delicate structures in the head from injury.
Mucosal surface area: These spaces provide a large surface area for the nasal mucosa, which helps to warm and humidify inhaled air.
The process of pneumatization can vary from person to person, which is why the size and shape of the mastoid air cells and paranasal sinuses can be different in different individuals. This is also why some people may be more prone to sinus infections than others.
Overall, pneumatization is a fascinating process that plays an important role in the development and function of the skull. It’s a testament to the amazing complexity and efficiency of the human body!
See more here: What Is The Theory Of Pneumatization Of The Mastoid? | Pneumatization Of Mastoid Air Cells Radiology
How symmetrical is the pneumatization of mastoid air cells?
To make sure our results were accurate, we didn’t include anyone who had previous medical or surgical problems in the area we were studying. This helped us to focus on the pneumatization of the mastoid air cells itself.
Pneumatization is the process of air-filled spaces forming in the bone. These spaces are called air cells. In the temporal bone, which is the bone that houses the ear, air cells can be found in the mastoid process. The mastoid process is the bony projection behind the ear.
The pneumatization of the mastoid air cells can vary from person to person. Some people have a lot of air cells, while others have very few. The size and shape of the air cells can also vary. This variation is usually symmetrical, meaning that the air cells on both sides of the head are roughly the same.
Pneumatization is important because it helps to protect the middle ear from infection. The air cells act as a buffer zone, preventing bacteria and other pathogens from reaching the middle ear. Pneumatization also helps to improve hearing by creating a better environment for sound waves to travel through.
While pneumatization is usually symmetrical, there are some cases where it is not. This can be caused by a number of factors, including:
Genetic predisposition: Some people are genetically predisposed to having asymmetrical pneumatization.
Previous ear infections: Repeated ear infections can damage the mastoid air cells, leading to asymmetrical pneumatization.
Surgery: Surgery on the mastoid bone can also affect pneumatization.
If you are concerned about the pneumatization of your mastoid air cells, you should talk to your doctor. They can perform a physical exam and order imaging tests, such as a CT scan, to assess the pneumatization of your mastoid air cells.
What are mastoid air cells?
These cells are pretty unique, though. They can vary a lot in size and how spread out they are. Some people might have a lot of these cells, while others have just a few. It all depends on how the mastoid bone developed.
Now, why are these mastoid air cells even there? They play a role in protecting your middle ear and helping to regulate pressure. You might be thinking, “How does a bunch of air pockets help with pressure?” Here’s the thing: Your middle ear needs to have the same air pressure as the outside world. Otherwise, you’d experience problems with your hearing. The mastoid air cells help balance this pressure. They connect to the middle ear through a small passageway, allowing air to flow between them.
Essentially, the mastoid air cells act like a little air-pressure regulator for your ears, keeping everything in balance for optimal hearing. Pretty cool, right?
Are mastoid air cells pneumatized?
Now, let’s talk about the other types. In a small percentage of cases, we observed either diploic or poorly pneumatized mastoid in 13 patients (8.7%). This means that the air spaces were either underdeveloped or partially filled with bone instead of air. Finally, only one Indian patient (0.7%) had sclerotic mastoid. This type is characterized by a very dense bone structure with minimal air spaces.
What are mastoid air cells and why are they important?
Mastoid air cells are interconnected air spaces within the mastoid bone, located behind the ear. They’re essentially extensions of the middle ear cavity. Their primary function is to lighten the skull, provide resonance for sound, and act as a buffer against infections. The presence of these air cells is crucial for normal hearing and protecting the delicate structures of the middle ear.
Pneumatization, which refers to the process of air filling these cells, is a complex process that starts during fetal development. A fully pneumatized mastoid is considered healthy and contributes to efficient sound transmission. On the other hand, poorly pneumatized or sclerotic mastoid can interfere with normal hearing, increase the risk of ear infections, and even lead to complications like mastoiditis. While the reasons behind variations in pneumatization are not fully understood, factors like genetics, age, and even environmental exposures are thought to play a role.
Do age-related studies influence the growth and development of mastoid air cells?
Mastoid air cells, also known as pneumatized cells, are air-filled spaces within the mastoid bone, located behind the ear. They develop during childhood and continue to grow throughout adolescence. The process of pneumatization, the formation of these air cells, is influenced by various factors, including genetics, environmental factors, and even the presence of infections. Age-related studies are crucial for understanding the development and growth of these air cells as they can provide insights into the natural process of temporal bone pneumatization.
These studies are important because they can help us understand how these air cells change over time, and how these changes might affect a person’s health. For example, if we know that air cells are more likely to become infected in older adults, we can develop strategies to prevent these infections.
Here’s how volumetric measurement can be used to study mastoid air cells:
CT Scans: CT scans are a great way to get detailed images of the mastoid bone. These images can then be used to create 3D models of the air cells.
Software Analysis: Special software programs can analyze the 3D models and calculate the volume of each air cell. This gives us a precise measurement of the size of the air cell system.
Data Collection: Researchers can collect data on the volume of air cells from a large group of people of different ages. This data can then be analyzed to see how the volume of air cells changes with age.
By conducting these age-related studies, researchers can gain a deeper understanding of the normal development of mastoid air cells and identify potential risk factors for ear infections and other health issues.
See more new information: countrymusicstop.com
Pneumatization Of Mastoid Air Cells Radiology | What Are Pneumatized Mastoid Air Cells?
So, what exactly is pneumatization?
Imagine a bunch of tiny air-filled spaces within the mastoid bone, right behind your ear. That’s what we’re talking about. These spaces, known as mastoid air cells, develop as you grow, and their size and shape can vary from person to person.
Radiology’s Role
Radiology plays a crucial role in understanding pneumatization because it allows us to visualize these air cells and assess their development. We’re not just looking at their presence, but also their size, shape, and any potential abnormalities.
Why is This Important?
Well, pneumatization patterns can give us clues about potential problems within the ear. For example:
Cholesteatoma: This is a growth of skin cells in the middle ear that can cause damage. Pneumatization can help us see if the air cells are affected, which can be a sign of this condition.
Otitis Media: This is a middle ear infection. The air cells can become filled with fluid, and imaging can help us see this.
Congenital Malformations: Sometimes, the air cells may not develop properly, which can be a sign of a birth defect.
Imaging Techniques
We typically use temporal bone CT (computed tomography) to visualize the mastoid air cells. This imaging technique gives us detailed cross-sectional views of the bone, allowing us to see the air cells in great detail.
What to Look for in Imaging
When we’re analyzing pneumatization on CT scans, we’re looking for:
Degree of Pneumatization: Is the mastoid bone well-pneumatized (full of air cells), partially pneumatized, or poorly pneumatized?
Air Cell Size and Shape: Are the air cells of normal size and shape, or are they abnormally large or small?
Presence of Abnormalities: Are there any signs of fluid within the air cells, bone erosion, or other abnormalities?
Interpreting the Images
Understanding pneumatization patterns is a skill that radiologists develop over time. They take into account all the factors I mentioned earlier, along with the patient’s clinical history and symptoms, to make a diagnosis.
FAQs
Q: What is the difference between a pneumatized and non-pneumatized mastoid bone?
A: A pneumatized mastoid bone has numerous air cells, while a non-pneumatized mastoid bone has very few or no air cells. This can be due to various factors, including genetics and ear infections.
Q: Can pneumatization change over time?
A: Yes, pneumatization can change over time, especially in children. Their mastoid air cells continue to develop as they grow.
Q: Does pneumatization affect hearing?
A: Yes, pneumatization can affect hearing. For example, if the air cells become filled with fluid, it can lead to conductive hearing loss.
Q: Can pneumatization be a sign of cancer?
A: It’s rare for pneumatization to be a direct sign of cancer, but imaging can sometimes help detect complications of ear cancer, such as bone erosion.
Q: What are the risks of mastoid surgery?
A: Mastoid surgery, like any surgery, carries some risks, including infection, bleeding, and hearing loss. The risks are usually low, but it’s important to discuss them with your doctor.
Conclusion
Pneumatization of mastoid air cells is a vital aspect of ear health, and radiology plays a crucial role in understanding this process. By analyzing the size, shape, and patterns of air cells, we can gain valuable insights into potential ear conditions and guide treatment decisions.
Remember, always consult with a qualified healthcare professional for any questions or concerns related to your health.
Hyperpneumatisation of mastoid air cells | Radiology
Excessive pneumatization of the mastoid air cells extending along occipital bone including condyle, clivus, and right petrous apex. Loculated and septated air collection Radiopaedia
Hypopneumatisation of the mastoid air cells | Radiology
Hypopneumatisation of the mastoid air cells is typically an anatomical variant. There may or may not be a link to otitis media with effusions in childhood. Radiopaedia
Pneumatization of the Mastoid | Radiology – RSNA
THIS communication purposes to trace the growth and development of the mastoid radiographically; to correlate roentgen findings to anatomic and clinical conceptions, RSNA Publications Online
Temporal bone pneumatization: A scoping review on the growth
Mastoid air cells in females was larger and increased significantly. However, among Bangele people of Indian, mastoid air cells increase by about 2 cm 2 every 5 National Center for Biotechnology Information
Pneumatization Pattern and Status of the Mastoid Antrum in
Epithelium infiltrates the growing bone and produces epithelium-lined air cell chambers, a process known as pneumatization. Conventional temporal bone National Center for Biotechnology Information
Temporal bone pneumatization: A scoping review on
In reporting the size of mastoid air cells across age groupings, 66.7% utilized area, 22.2% utilized volume, while 11.1% utilized both area and volume. Findings from this review showed that the plos.org
Pneumatization of Mastoid Air Cells, Temporal Bone, Ethmoid
The PNS and other parts of temporal bone like mastoid air cells system have been found to have multiple functions including humidification, adding resonance National Center for Biotechnology Information
Imaging Review of the Temporal Bone: Part I. Anatomy
When present, petrous apex air cells are connected to the mastoid air cells via numerous supra- and infralabyrinthine air channels that facilitate spread of infection from the mastoid air cells and middle RSNA Publications Online
Computed Tomography of Temporal Bone Pneumatization: 1.
The pneumatization of 141 “normal” temporal bones on computed tomography (CT) was evaluated in 100 patients (age range, 6-85 years), Because of the controversy American Journal of Neuroradiology
Mastoidectomy Anatomy
Acute Otomastoiditis | Ct Scan |Radiology |
Otomastoiditis Summary – Middle Ear Mri – Mri Online
Anatomy Of The Temporal Bone On Imaging
How To Read Temporal Bone Imaging!
Link to this article: pneumatization of mastoid air cells radiology.
See more articles in the same category here: blog https://countrymusicstop.com/wiki
