What does a PETCO2 of 8 mm/hg mean?
A low PETCO2 level could mean a few things. It could be that the patient has a low amount of carbon dioxide in their blood, which might indicate that their breathing is not effective. It could also mean that the circulation is not strong enough to deliver oxygenated blood to the lungs.
Here’s what you need to know:
PETCO2 stands for “end-tidal carbon dioxide”, which is the amount of carbon dioxide in the exhaled breath.
Normal PETCO2 levels are typically between 35 and 45 mm Hg.
A low PETCO2 level can be a sign that the patient’s circulation is poor, which can happen when chest compressions are not effective.
It’s important to reassess your chest compression technique and ensure you’re delivering effective compressions.
While a low PETCO2 is a concern, it’s crucial to stay calm and continue ventilating and performing chest compressions.
Remember, the capnography screen is a valuable tool that can help you monitor the effectiveness of your CPR efforts. If the PETCO2 remains low, you may need to adjust your technique or seek assistance from a more experienced provider.
What should PETCO2 be during CPR?
High-quality chest compressions are very important, and one way to measure their effectiveness is by looking at the ETCO2 value. You want to see an ETCO2 of 10 to 20 mmHg.
When the heart starts beating again (we call this ROSC, or return of spontaneous circulation), you’ll see a big increase in the ETCO2. Think of it like this: the ETCO2 will go up to 35 to 45 mmHg. This is a good thing because it means that blood is flowing much better, and the body is getting the oxygen it needs.
Here’s a little more about what’s going on with ETCO2 during CPR:
ETCO2 stands for end-tidal carbon dioxide, and it’s a measurement of the amount of carbon dioxide in the air you exhale. It’s a really useful tool for CPR because it tells us how well the blood is circulating.
During CPR, the heart isn’t pumping blood around the body, so we’re relying on the chest compressions to move the blood. When the blood gets to the lungs, it releases carbon dioxide. The more blood that reaches the lungs, the higher the ETCO2 reading.
So, a good ETCO2 reading during CPR means that your compressions are working and that blood is circulating to the lungs. It also tells us that the patient has a better chance of survival.
What capnography shows a persistent waveform and a PETCO2 of 8?
While a PETCO2 of 8 might seem low, it’s important to remember that during CPR, the blood flow to the lungs is significantly reduced. This means that the amount of carbon dioxide being exhaled is also reduced. Therefore, a low PETCO2 reading is not necessarily a bad thing.
It’s essential to consider the overall context of the situation. If the waveform is persistent and the PETCO2 is stable, it suggests that the chest compressions are generating adequate blood flow, even though it’s much lower than normal. However, a fluctuating waveform or a declining PETCO2 might indicate a problem with the chest compressions or other factors, and a reevaluation of the CPR technique is necessary.
It’s also important to note that a PETCO2 reading alone cannot be used to diagnose the effectiveness of CPR. Other factors, such as the patient’s response to CPR, the quality of the compressions, and the presence of other medical conditions, must be considered.
Here’s a breakdown of what this means:
Persistent waveform: This indicates that the endotracheal tube is in place and that air is moving through the lungs.
PETCO2 of 8: This is a relatively low reading, but it is not necessarily a cause for concern during CPR. It simply means that the amount of carbon dioxide being exhaled is reduced due to the limited blood flow to the lungs.
In summary, a persistent waveform and a PETCO2 of 8 during CPR is a positive sign indicating effective chest compressions. However, it’s crucial to monitor the waveform and PETCO2 levels closely and adjust CPR techniques as needed.
What is the normal Petco range?
Let’s dive deeper into this: PetCO2 is a non-invasive way to monitor your pet’s respiratory health. It’s a great tool for veterinarians to use because it can provide a quick and easy way to assess how well your pet’s lungs are functioning. A PetCO2 reading can tell us if your pet is breathing too fast or too slow, if their blood isn’t getting enough oxygen, or if there’s a problem with their lungs.
But why is the PetCO2 range the same as the arterial blood gas range? It’s because the CO2 levels in your pet’s exhaled breath are directly related to the CO2 levels in their blood. This means that the PetCO2 reading can be a good indicator of the CO2 level in the blood.
However, it’s important to remember that PetCO2 is just one piece of the puzzle when it comes to assessing your pet’s respiratory health. It’s always best to discuss your pet’s health with your veterinarian, as they can consider all of the factors involved, including the PetCO2 reading, to provide the best possible care for your furry friend.
What is a high-quality CPR?
Chest compression fraction should be greater than 80%. This means that you should be compressing the chest more than you’re not. In other words, you should be compressing the chest for at least 80% of the time during a CPR cycle.
Compression rate should be between 100 and 120 compressions per minute. This is a good pace to get blood flowing.
Compression depth is important, too. For adults, we’re looking for at least 50 millimeters (2 inches). For infants and children, the depth should be at least one-third of the anterior-posterior (AP) dimension of the chest.
So, what does this all mean? Well, it means that when you’re doing CPR, you’re giving the heart the best chance to keep pumping blood. You’re not just pushing on the chest; you’re actively trying to help the heart do its job.
Think of it like this: imagine you’re trying to start a car with a dead battery. You could just push on the gas pedal, but that won’t get the engine running. You need to use jumper cables to give the battery a jump start. In the same way, CPR is like giving the heart a jump start. You’re not just pushing on the chest; you’re giving the heart the extra boost it needs to get back to work.
High-quality CPR is about more than just doing the movements; it’s about understanding the science behind it. By following these guidelines, you can make sure you’re giving the person you’re helping the best possible chance of survival.
What is a good ETCO2 for CPR?
Ideally, you want to see an ETCO2 of at least 20 mmHg during CPR, and even better, greater than 20 mmHg. Why? Because this means that your compressions are generating enough blood flow to the lungs to produce a decent amount of CO2.
Think of it like this: normal ETCO2 is around 35-45 mmHg. During CPR, you’re aiming for about 1/4 of that, which is about 10-15 mmHg. This means that the heart, even though it’s not beating properly, is still pumping some blood through the body, which is a good sign!
But why 1/4? This is because CPR aims to deliver roughly 1/4 of normal cardiac output. This means that even though the heart isn’t working properly, your compressions are effectively keeping blood flowing.
Here’s a simple way to think about it:
Lower ETCO2: This means the blood flow is low. You need to check your technique and make sure you’re doing proper chest compressions.
Higher ETCO2: This means the blood flow is good, and you’re doing a great job!
Remember, ETCO2 is just one tool to help you measure the effectiveness of CPR. It’s important to use it along with other indicators like pulse and rhythm to get a complete picture of the patient’s condition.
Let’s dive deeper into the why behind the numbers:
Imagine you’re trying to push a car up a hill. The more forcefully you push, the further the car moves. In CPR, the force of your compressions is like pushing the car. The further the car moves (the better the blood flow), the more CO2 it produces.
So, a higher ETCO2 means you’re generating enough force to push a decent amount of blood through the body. This is a good thing!
However, don’t let a lower ETCO2 discourage you. It just means you need to adjust your technique to improve the blood flow. There are many things you can do, like:
Make sure you’re compressing deep enough: You want to compress the chest about 2 inches (5 cm) for adults.
Compress at the right rate: Aim for 100-120 compressions per minute.
Minimize interruptions: Try to minimize breaks in compressions to keep the blood flowing.
By keeping track of ETCO2 and making adjustments as needed, you can ensure that you’re providing the best possible care for your patient.
What rate should CPR be?
When performing CPR, it’s essential to maintain a consistent and effective compression rate. Think of it like a steady rhythm. If you’re compressing too slowly, you’re not giving the heart enough help to pump blood. But if you’re compressing too quickly, you might not allow the chest to fully recoil, reducing the effectiveness of each compression.
The American Heart Association’s suggestion of using the song Stayin’ Alive is a great way to get a feel for the correct pace. The song’s tempo is right around 100 to 120 beats per minute, which is the ideal rate for CPR compressions. However, you don’t have to be singing along to get it right! Just try to keep a consistent rhythm that mirrors the song.
Remember, even though the American Heart Association has established this recommended pace, there may be variations depending on the situation. Ultimately, the goal is to provide adequate blood flow to the brain and other vital organs, so adjust your pace as needed to achieve that.
Why is ETCO2 low during CPR?
Think of ETCO2 as a window into what’s happening in the body during CPR. It’s like a little gauge telling us how well the heart is working. When ETCO2 is low, it means that the heart isn’t pumping effectively, and the blood isn’t carrying enough carbon dioxide out of the body. This can be caused by a few different things.
First, poor compressions mean that the heart isn’t getting the right amount of pressure to pump blood around the body. Think of it like a squeezing a water balloon – if you don’t squeeze it hard enough, you won’t get much water out! Poor compressions mean that not enough blood is being pumped to the lungs to exchange oxygen and carbon dioxide.
Next, if the heart has been stopped for a long time, or if the body is in shock, it can affect the ability of blood to flow to the tissues. This is because the body’s cells are not getting the oxygen they need to function properly, so they can’t get rid of carbon dioxide as efficiently.
So, when ETCO2 is low during CPR, it’s a sign that the body isn’t getting the oxygen it needs and that the heart is not pumping efficiently. This is a very serious situation, and it’s important to act quickly to improve the situation. By improving the quality of compressions and addressing the underlying cause of the low ETCO2, it’s possible to give the body a better chance of recovery.
What is the main determinant of PetCO2 during CPR?
A persistently low PetCO2 level during CPR, particularly below 10 mm Hg in intubated patients, can be an important indicator of the likelihood of achieving return of spontaneous circulation (ROSC). However, it’s vital to remember that PetCO2 is just one piece of the puzzle, and other factors like chest compressions quality and rhythm, the presence of a defibrillation-able rhythm, and the underlying cause of the arrest also play a significant role in determining the outcome.
PetCO2 can be a valuable tool for monitoring the effectiveness of CPR. If PetCO2 levels remain consistently low, it may suggest that the current CPR efforts are not effective in delivering sufficient blood to the lungs. This might prompt the healthcare team to re-evaluate their CPR technique, assess the need for additional medications, or consider alternative strategies to improve blood flow.
However, it’s crucial to interpret PetCO2 levels in the context of the overall clinical picture. A low PetCO2 doesn’t automatically mean that ROSC is unlikely. Other factors might be contributing to the low PetCO2, and other vital signs should be monitored as well. The healthcare team should carefully consider all aspects of the patient’s condition and the ongoing CPR efforts to make informed decisions about the best course of action.
What is the level of PetCO2 in ACLS?
PetCO2 stands for “Partial Pressure of Carbon Dioxide” in Expired Air. Think of it as a window into the carbon dioxide levels in your patient’s blood. During ACLS, we often use quantitative waveform capnography to measure this PetCO2. It’s a very important tool to assess how well the lungs are working and how effectively the patient is breathing.
In ACLS, we aim for a PetCO2 between 35-40 mm Hg. This range indicates good gas exchange and appropriate oxygenation in the body. If the PetCO2 is too high, it means the patient is not breathing out enough carbon dioxide. This could be due to a number of factors like poor ventilation, airway obstruction, or even lung disease. On the other hand, if PetCO2 is too low, it might signal hyperventilation or other issues.
How do we manage this? Well, if you have access to a capnography machine, you can titrate the oxygen to maintain that optimal PetCO2 range. This means adjusting the oxygen flow rate up or down to achieve the desired PetCO2 level. It’s a bit like fine-tuning an instrument! If you don’t have capnography available, you can still monitor oxygen saturation with a pulse oximeter. Aim for a saturation between 92-98%.
But why is PetCO2 so important in ACLS?
It’s a vital indicator of how effectively the heart and lungs are working together. PetCO2 helps us assess the effectiveness of our interventions, like ventilation and oxygen therapy. For example, if we are ventilating a patient and the PetCO2 is not changing, it might indicate that the ventilation is not working properly. Or, if the PetCO2 is decreasing, it might mean that the ventilation is becoming too effective and could lead to hyperventilation.
Remember, PetCO2 is a dynamic measurement. It changes constantly in response to the patient’s condition. So, we need to keep a close eye on it to ensure that our treatment plan is working and adjusting as needed.
See more here: What Should Petco2 Be During Cpr? | Petco2 Of 8 During Cpr
What should be the Petco2 level during CPR?
During CPR, aiming for a PetCO2 level of 20 mmHg or higher is a good target. This means you’re getting good quality compressions and blood flow. Remember, consistent CPR is key to successful resuscitation. Continuous capnography, which measures the carbon dioxide in exhaled breath, can help you keep track of your compressions and make sure they’re strong and steady.
But why is PetCO2 so important during CPR? Think of it as a window into what’s happening inside the body during this crucial time. When you’re performing CPR, you’re essentially taking over the role of the heart, forcing blood to circulate. A higher PetCO2 reading means the blood is moving through the lungs more effectively, which is a good sign that your compressions are doing their job. If the PetCO2 is low, it could indicate poor circulation or that the compressions aren’t effective enough.
Here’s a quick breakdown:
Higher PetCO2 levels during CPR mean your compressions are effective and the blood is being circulated well.
Lower PetCO2 levels might mean your compressions aren’t strong enough or that there’s some other issue with blood circulation.
So, how do you get that PetCO2 level up?
The key is consistent, high-quality compressions. Think about these factors:
Depth: Aim for about 2 inches of chest compression depth for an adult.
Rate: Around 100 to 120 compressions per minute.
Avoid interruptions: Keep those compressions going! Limit pauses between compressions as much as possible.
Capnography is like having a built-in monitor for your compressions. It can help you make adjustments to your technique in real time.
Remember, the ultimate goal of CPR is to restore blood flow to the brain and other vital organs. A PetCO2 level of 20 mmHg or higher is a good sign that your CPR efforts are on the right track.
Can capnography predict CPR outcomes based on Petco 2 values?
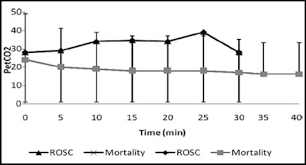
A sudden increase in PetCO2 values is a promising sign during CPR. It suggests that the heart has started beating again, also known as return of spontaneous circulation (ROSC). This is because as the heart begins to circulate blood effectively, the lungs are able to eliminate carbon dioxide more efficiently.
Capnography is becoming increasingly common during CPR. As more data is collected, we have a great opportunity to study the relationship between PetCO2 values and CPR outcomes. This could lead to better predictions about which patients are most likely to survive CPR and which CPR strategies are most effective.
Here’s how capnography can predict CPR outcomes:
Early detection of ROSC: A rapid increase in PetCO2 values is a strong indicator of ROSC. This early detection can allow healthcare providers to adjust their CPR strategies and optimize resuscitation efforts.
Monitoring the effectiveness of CPR:PetCO2 values can also provide information about how well CPR is working. For example, if PetCO2 values remain low or decrease, it may indicate that CPR is not effective and that adjustments are needed.
Identifying patients who are less likely to survive:PetCO2 values can help predict which patients are less likely to survive CPR. For example, patients with consistently low PetCO2 values during CPR may have a lower chance of survival.
Guiding resuscitation strategies:Capnography can help guide resuscitation strategies. For example, if PetCO2 values are low, providers may use a different ventilation strategy or increase chest compression depth to improve blood flow.
While capnography is a valuable tool, it’s important to remember that it is just one piece of the puzzle in predicting CPR outcomes. Other factors such as the patient’s underlying health conditions, the duration of CPR, and the quality of CPR performed also contribute to the likelihood of survival.
As more data is collected and analyzed, our understanding of the role of capnography in CPR will continue to grow. This will lead to even better ways to use this tool to improve patient outcomes.
Is there a correlation between cardiac output and petco2?
It’s been found that there’s a positive correlation between cardiac output and PetCO2 (end-tidal carbon dioxide). This discovery has led to the widespread use of capnography in cardiac arrest situations.
Capnography is a monitoring technique that measures the amount of carbon dioxide in the exhaled breath. This measurement can help us understand how well the heart is pumping blood and delivering oxygen to the body. When the heart stops, as in cardiac arrest, the blood flow to the lungs also stops. This means no carbon dioxide is being delivered to the lungs to be exhaled. So, the PetCO2 value drops to zero very quickly.
Think of it like this: When you exhale, you’re getting rid of waste products like carbon dioxide. This waste is carried from your tissues by the blood and delivered to your lungs to be exhaled. The cardiac output is a measure of how much blood your heart pumps in one minute. If your heart stops, your cardiac output drops to zero. As a result, there’s no blood flowing through your lungs to deliver carbon dioxide for exhalation.
This is why capnography is so important in cardiac arrest situations. By monitoring the PetCO2 value, we can get an indication of whether the heart is pumping blood and delivering oxygen to the body.
So, if we see a decrease in PetCO2 during CPR, it’s a sign that the chest compressions are not effective in restoring blood flow to the lungs. This means that we need to adjust our CPR techniques to improve the effectiveness of blood circulation.
It is important to note that this correlation is not absolute and can be influenced by other factors, such as ventilation and lung function. However, it provides valuable insights into the effectiveness of CPR and helps guide resuscitation efforts.
Can Petco 2 help in refractory cardiac arrest?
PETCO2 is a measure of carbon dioxide in exhaled breath. In patients with RCA, the heart is unable to pump blood effectively, leading to a buildup of carbon dioxide in the body. This buildup can be detected by capnography, which can help clinicians assess the severity of the RCA.
When PETCO2 levels are high, it can indicate that the patient is not getting enough oxygen and that their body is struggling to remove carbon dioxide. This can be a sign that the patient is at risk of death and may benefit from ECLS. ECLS is a life support system that can take over the function of the heart and lungs, giving the body time to recover.
There is a growing body of research that suggests that using PETCO2 as a guide for initiating ECLS in patients with RCA can improve outcomes. However, it is important to note that PETCO2 is just one factor to consider when making decisions about ECLS. Other factors, such as the patient’s age, medical history, and overall health, will also be taken into account.
ECLS is a complex procedure with risks and benefits, and it is important to discuss all of these with your healthcare provider before making any decisions about treatment.
See more new information: countrymusicstop.com
Petco2 Of 8 During Cpr: What Does It Mean?
You’re in the middle of a code, and you’re monitoring the patient’s vital signs. You see the PetCO2 reading on the monitor, and it’s at 8. Your heart sinks. What does this mean, and what should you do?
Let’s break down what a PetCO2 of 8 means, why it’s a big deal during CPR, and the steps you can take to address this critical situation.
Understanding PetCO2
PetCO2, or end-tidal carbon dioxide, is a measurement of the amount of carbon dioxide in the exhaled breath. It’s a reliable indicator of how well the body is ventilating and how effectively the lungs are removing carbon dioxide from the bloodstream.
During CPR, a normal PetCO2 reading would be between 35 and 45 mmHg. A PetCO2 of 8 is significantly low, suggesting a serious problem with oxygen delivery and carbon dioxide elimination.
Why a PetCO2 of 8 is a Red Flag During CPR
Think of it like this: when your body is working properly, your lungs act like a pump, removing carbon dioxide waste from your blood and sending in fresh oxygen. During CPR, the heart isn’t pumping blood, and the lungs aren’t getting enough oxygen in. This can lead to a buildup of carbon dioxide in the blood, and a low PetCO2 reading is a sign that things are not going well.
Causes of Low PetCO2 During CPR
Here are some of the main culprits behind a low PetCO2 reading during CPR:
Poor Chest Compressions: Inadequate compressions can lead to poor blood circulation and ineffective removal of carbon dioxide from the body.
Inadequate Ventilation: If the person is not being properly ventilated during CPR, they are not getting enough oxygen, and carbon dioxide builds up.
Underlying Medical Condition: The person might already be struggling with a medical condition that impacts breathing or blood circulation, making it harder to revive them.
Respiratory Failure: The person’s respiratory system might have failed, making it impossible for them to breathe effectively, even with CPR support.
What to Do When You See a PetCO2 of 8
It’s important to remember that a low PetCO2 reading during CPR is a serious sign, and action needs to be taken quickly. Here’s a breakdown of steps to take:
1. Double-Check Your Technique: Ensure that your chest compressions are effective and that the person is getting proper ventilation.
Chest compressions: Make sure they are deep and fast, at a rate of 100 to 120 per minute. Ensure you’re compressing the chest to at least 2 inches deep.
Ventilation: Confirm that you are providing adequate ventilation, making sure the chest rises with each breath.
2. Consider Advanced Life Support (ALS) Measures: Depending on the situation and your role, you might need to consider initiating ALS measures like intubation or medication to improve ventilation and circulation. These measures are typically done by paramedics or other trained medical professionals.
3. Don’t Give Up: Remember, a low PetCO2 reading doesn’t mean the person is beyond help. Continue CPR and other supportive measures while working with the medical team.
Improving CPR Outcomes: Beyond PetCO2
While PetCO2 is a critical factor in assessing the effectiveness of CPR, it’s not the only one. Here are some additional tips to enhance your CPR skills and increase the chances of a successful outcome:
Practice Regularly: Regular CPR training and practice sessions can help you develop the skills and confidence to deliver effective CPR in an emergency.
Use a High-Quality CPR Device: Using a high-quality CPR device, such as an automated external defibrillator (AED), can significantly improve the effectiveness of chest compressions and enhance the chances of survival.
Follow CPR Guidelines: Stay updated on the latest CPR guidelines and recommendations. These guidelines are constantly evolving and can improve your ability to deliver effective CPR.
FAQs about PetCO2 During CPR
Q: What does a low PetCO2 reading during CPR mean?
A: A low PetCO2 reading during CPR typically indicates that the body is not effectively removing carbon dioxide from the bloodstream, which may be due to poor circulation, inadequate ventilation, or an underlying medical condition.
Q: What are the common causes of low PetCO2 during CPR?
A: The most common causes include inadequate chest compressions, ineffective ventilation, pre-existing medical conditions, and respiratory failure.
Q: What should I do if I see a low PetCO2 reading during CPR?
A: It’s important to take immediate action. Double-check your CPR technique, consider ALS measures, and continue CPR and other supportive measures while working with the medical team.
Q: Can I use PetCO2 to predict the outcome of CPR?
A:PetCO2 can be a valuable indicator of CPR effectiveness, but it’s not a guaranteed predictor of outcome. Other factors, such as the underlying medical condition, the duration of cardiac arrest, and the quality of CPR also play a role.
Q: What is the ideal PetCO2 reading during CPR?
A: While an ideal PetCO2 reading during CPR isn’t a definitive benchmark, a reading above 35 mmHg generally suggests adequate blood circulation and ventilation.
Remember, a low PetCO2 reading is a serious sign that requires immediate attention. By understanding the implications of low PetCO2 and following appropriate steps, you can help increase the chances of a successful outcome during CPR.
Capnography during cardiopulmonary resuscitation: Current
The height of the CO 2 waveform during CPR, which is a function of cardiac output during chest compression, should be monitored, and every effort should be made National Center for Biotechnology Information
Capnography During Cardiopulmonary Resuscitation
In the acute settings, for a given ventilation, PETCO2 is function of cardiac output (pulmonary perfusion). This is the basic principle of directing the uses of capnography Capnography
Capnography in Cardiac Arrest • LITFL • CCC Resuscitation
Current ILCOR guidelines advise that capnography is useful during cardiac arrest resuscitation; ETCO2 can be used as a surrogate marker of cardiac output; Life in the Fast Lane
Capnography during cardiac arrest – Resuscitation
Measurement of end-tidal expiratory pressure of carbon dioxide (ETCO 2) using capnography provides a noninvasive estimate of cardiac output and organ perfusion during cardiac arrest and can Resuscitation
CAPNOGRAPHY: MEASURING END-TIDAL CO LEVELS
2 value (< 10 mmHg) during CPR in an intubated patient suggests that the quality of chest compressions needs improvement. •Ensure proper rate (approximately 100/min) Mount Sinai Health System
Comparison of end-tidal carbon dioxide levels with
When ventilations are provided without chest compressions during CPR, the PetCO2 levels reach down to zero after some time. Increase in pulmonary perfusion National Center for Biotechnology Information
Capnography during cardiopulmonary resuscitation: Current
There is emerging evidence that PETCO2 values can guide the initiation of extracorporeal life support (ECLS) in refractory cardiac arrest (RCA). There is also increasing PubMed
Cardiac output and PETCO2 – Capnography
A PETCO2 greater than 30 mm Hg was invariably associated with a cardiac output more than 4 L/min or a cardiac index > 2 L/min.5 Furthermore, when PETCO2 Capnography
Capnography In Cardiac Arrest
Nursing Skills For Doctors: Setting Up The End Tidal Co2 Monitor
Waveform Capnography
E-Learning: Basics Of Capnography
How To Set Up: Etco2 Monitoring
Link to this article: petco2 of 8 during cpr.
See more articles in the same category here: blog https://countrymusicstop.com/wiki
